The neurodevelopmental illness known as Attention Deficit Hyperactivity illness (ADHD) is marked by recurrent patterns of hyperactivity, impulsivity, and inattention that seriously hinder day-to-day functioning. Although the behavioral symptoms of ADHD have long been known, our knowledge of the underlying neurological pathways is still developing. Advances in neuroscience have illuminated the complex interactions between different brain regions, neurotransmitter systems, and genetic variables that contribute to the development of ADHD. The neurobiology of ADHD is examined in this article, which includes the most recent research discoveries and their implications for diagnosis, treatment, and public perception of this widespread condition.
Brain Regions and Neural Circuits Associated with ADHD
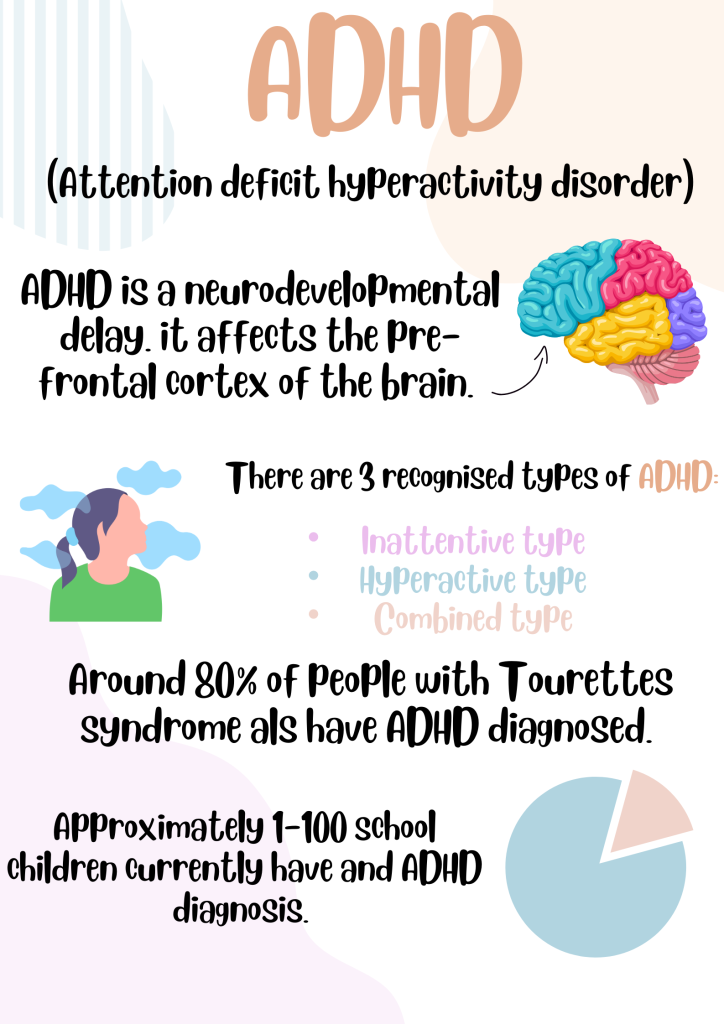
Research employing neuroimaging methods like positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) has yielded important insights into the neurological basis of ADHD. The disruption of brain networks related to motor activity, impulse control, and attention is one of the main discoveries. The prefrontal cortex (PFC), basal ganglia, cerebellum, and anterior cingulate cortex (ACC) are important brain areas associated with ADHD.
Executive functions like working memory, cognitive regulation, and decision-making are significantly influenced by the prefrontal cortex (PFC), specifically the dorsolateral prefrontal cortex (DLPFC) and the ventrolateral prefrontal cortex (VLPFC). Deficits in sustained attention and impulse control that are seen in ADHD patients have been linked to dysfunction in these regions.
The striatum and the nucleus accumbens are two examples of the structures that make up the basal ganglia, which are responsible for controlling motor behavior and reward processing. The impulsivity and hyperactivity that characterize ADHD have been linked to changes in dopaminergic transmission in the basal ganglia.
Traditionally recognized for its function in motor coordination, the cerebellum has also been linked to attentional regulation and cognitive processes. People with ADHD have been shown to have abnormalities in the structure and connectivity of the cerebellum, which may indicate that the pathophysiology of the condition involves the cerebellum.
Those with ADHD have altered activity and connection patterns in the ACC, an area linked to error monitoring and conflict resolution. Difficulties properly managing attentional resources and suppressing incorrect reactions may be related to dysfunction in the ACC.
Systems of Neurotransmitters: Beyond Dopamine
Dopamine has long been linked to ADHD. It is a neurotransmitter that is involved in motivation, reward processing, and motor control. According to the dopamine hypothesis, one of the main causes of the symptoms of ADHD is a disruption of dopamine signaling, namely in the mesocorticolimbic circuit. Variations in the genes producing dopamine receptors and transporters have been linked to an increased risk of ADHD, according to genetic studies.
But dopamine is not the only neurotransmitter system involved in ADHD neurobiology; norepinephrine, serotonin, and glutamate are also involved. Norepinephrine is involved in the control of arousal and attention, and drugs that block norepinephrine reuptake are effective in treating ADHD. ADHD symptoms such as emotional dysregulation and impulsivity have been associated with serotonin deficiency. The main excitatory neurotransmitter in the brain, glutamate, influences synaptic plasticity and may have a role in the cognitive abnormalities associated with ADHD.
Environmental and Genetic Factors
It is widely acknowledged that ADHD is a highly heritable illness, with genetic variables thought to account for 70–80% of the variation in ADHD liability. Numerous genetic risk loci linked to ADHD have been found through genome-wide association studies (GWAS); many of these loci are related to neuronal development, dopamine signaling, and synaptic function. That being said, ADHD is regarded as a polygenic disorder, meaning that multiple genes each have a tiny effect on the total risk.
ADHD risk and severity are significantly shaped by environmental factors in addition to genetic factors. ADHD risk has been associated with prenatal exposure to maternal smoking, alcohol consumption, or use of specific drugs. ADHD symptoms can also arise as a result of adverse childhood experiences, such as early trauma, neglect, or ongoing stress. Deciphering the intricate etiology of ADHD necessitates an understanding of the interaction between genetic predispositions and environmental influences.
Implications for Treatment and Diagnosis
The diagnosis and treatment of ADHD are significantly impacted by the neurological understanding of the disorder. The objective assessment of ADHD and its distinction from other psychiatric diseases with overlapping symptoms may be facilitated by neuroimaging biomarkers. For instance, quantitative measurements of the structure and function of the brain may enhance diagnostic precision and be used in conjunction with conventional behavioral evaluations.
Additionally, pharmaceutical therapies that specifically target particular neurotransmitter systems have been developed as a result of our growing understanding of the neurochemical foundations of ADHD. Among the best therapies for ADHD are stimulant drugs, such amphetamine and methylphenidate, which improve dopamine and norepinephrine signaling. For those who are intolerant of stimulant side effects or do not respond to stimulants, non-stimulant drugs like atomoxetine and guanfacine act on the norepinephrine and noradrenergic receptors.
Behavioral therapies and psychosocial support are essential for controlling symptoms of ADHD and enhancing functional outcomes, in addition to medication. Individuals with ADHD can benefit from school adjustments, parent education, and cognitive-behavioral therapy (CBT) in order to improve their academic performance, acquire coping mechanisms, and become more organized.
Final Thoughts
The intricate interaction of genetic, neurochemical, and environmental elements that characterizes the neurobiology of ADHD contributes to the disorder’s variable presentation in different people. Our understanding of the etiology and pathophysiology of ADHD has deepened thanks to developments in neuroimaging, molecular genetics, and systems neuroscience. This has opened the door to more individualized approaches to diagnosis and treatment.
Going forward, solving the remaining puzzles surrounding ADHD and creating more specialized treatments will require collaborative research projects combining genetics, neurology, and clinical psychology. Understanding the brain processes that underlie ADHD will help us to better understand the illness, lessen stigma around it, and enable those who are impacted by it to succeed in both the social and academic spheres.