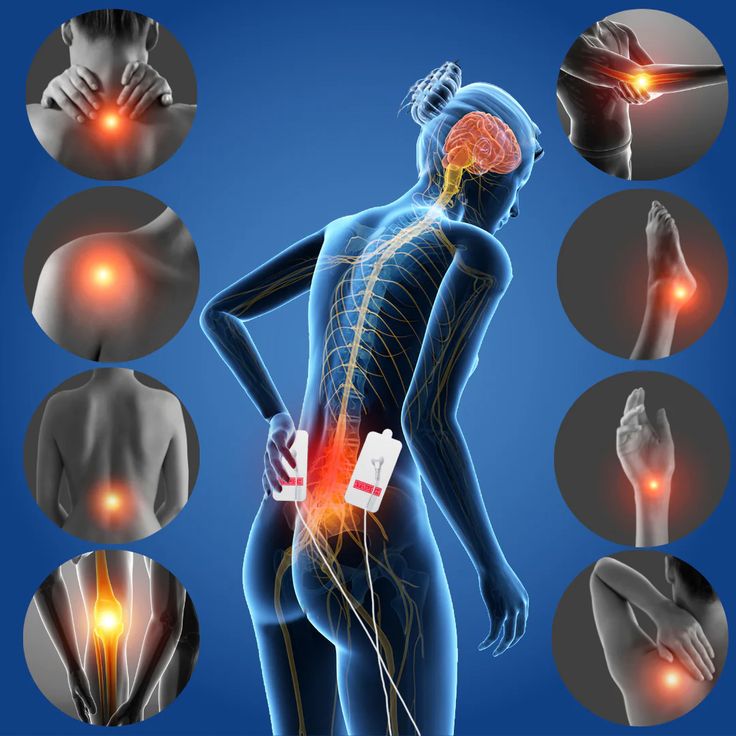
Chronic pain is a complex and multifaceted condition that can significantly impact quality of life. Exploring the science behind chronic pain involves understanding its underlying mechanisms and exploring various treatment options. Here’s an overview:
Aspadol 200mg tablets treat moderate to severe levels of pain in case of both acute and chronic musculoskeletal pain in a person, whether it is by injury or surgery. Also, it is used when round-the-clock medication is the priority, and one needs to control the pain of diabetic nephropathy.Common side effects of this drug are counted as follows. There’s not much to worry about, but if the problem persists for long, seek medical Help.
Mechanisms of Chronic Pain:
- Peripheral Sensitization: Chronic pain often begins with tissue damage or inflammation. Persistent nociceptive input from damaged tissues can lead to sensitization of peripheral nerves, resulting in increased pain sensitivity and amplification of pain signals.
- Central Sensitization: Prolonged nociceptive input can also lead to central sensitization, characterized by heightened sensitivity of neurons in the central nervous system (CNS), particularly in the spinal cord and brain. Central sensitization can result in exaggerated responses to painful stimuli and the development of widespread pain hypersensitivity.
- Neuroplastic Changes: Chronic pain is associated with neuroplastic changes in the CNS, including alterations in synaptic connectivity, neurotransmitter function, and gene expression. These changes can perpetuate and exacerbate pain, contributing to the persistence of chronic pain states.
- Inflammatory Processes: Inflammation plays a significant role in many chronic pain conditions, such as arthritis, fibromyalgia, and inflammatory bowel disease. Dysregulated immune responses and inflammatory mediators contribute to tissue damage, sensitization of nociceptive pathways, and the maintenance of chronic pain.
- Psychosocial Factors: Psychological and social factors, including stress, anxiety, depression, trauma, and social isolation, can influence the perception and experience of pain. Chronic pain often coexists with mental health disorders and psychosocial stressors, which can exacerbate pain symptoms and contribute to functional impairment.
Treatment Options for Chronic Pain:
- Medications: Pharmacological treatments for chronic pain include analgesics (e.g., nonsteroidal anti-inflammatory drugs [NSAIDs], opioids, acetaminophen), adjuvant medications (e.g., antidepressants, anticonvulsants, muscle relaxants), and topical agents (e.g., lidocaine patches, capsaicin cream). Medication selection depends on the type and severity of pain, as well as individual patient factors.
- Physical Therapy: Physical therapy interventions, such as exercise, stretching, manual therapy, and modalities (e.g., heat, cold, electrical stimulation), can improve mobility, strength, flexibility, and function, reduce pain intensity, and promote overall well-being.
- Psychological Therapies: Psychological interventions, including cognitive-behavioral therapy (CBT), mindfulness-based therapies, relaxation techniques, and stress management strategies, can help individuals cope with chronic pain, reduce pain-related distress, and improve psychological functioning.
- Interventional Procedures: Interventional procedures, such as nerve blocks, epidural injections, radiofrequency ablation, and spinal cord stimulation, can provide targeted pain relief by interrupting pain signals or modulating neural activity in specific pain pathways.
- Complementary and Integrative Therapies: Complementary and integrative therapies, including acupuncture, chiropractic care, massage therapy, biofeedback, and herbal supplements, may offer additional options for managing chronic pain, although evidence of their effectiveness varies.
- Lifestyle Modifications: Lifestyle modifications, such as optimizing sleep hygiene, maintaining a healthy diet, managing stress, engaging in regular physical activity, and avoiding tobacco and excessive alcohol consumption, can complement other pain management strategies and promote overall health and well-being.
- Multidisciplinary Pain Management: Multidisciplinary pain management programs integrate various treatment modalities, including medical, rehabilitative, psychological, and complementary approaches, within a coordinated care framework. These programs aim to address the complex biopsychosocial factors contributing to chronic pain and optimize treatment outcomes.
- Innovative Therapies: Emerging treatments for chronic pain include neuromodulation techniques (e.g., transcranial magnetic stimulation, dorsal root ganglion stimulation), regenerative medicine approaches (e.g., stem cell therapy, platelet-rich plasma injections), and novel pharmacological agents targeting specific pain pathways or mechanisms.
Challenges in Chronic Pain Management:
- Individual Variability: Chronic pain is a highly individualized condition, and treatment responses vary among individuals. Personalized approaches to pain management that consider patient preferences, comorbidities, psychosocial factors, and treatment goals are essential.
- Risk-Benefit Balance: Many pharmacological treatments for chronic pain, such as opioids and certain adjuvant medications, carry risks of adverse effects, dependence, misuse, and overdose. Clinicians must carefully weigh the potential benefits and risks of treatment options and engage in shared decision-making with patients.
- Access to Care: Disparities in access to comprehensive pain management services, including specialty care, interdisciplinary pain programs, and nonpharmacological treatments, pose significant challenges for individuals with chronic pain, particularly in underserved populations.
- Stigma and Misconceptions: Stigma surrounding chronic pain, opioid use, and mental health disorders can contribute to undertreatment, social isolation, and barriers to seeking help. Education, advocacy, and destigmatization efforts are needed to promote compassionate and evidence-based approaches to pain care.
- Integration of Care: Fragmentation of care and lack of coordination among healthcare providers can impede the delivery of comprehensive and holistic pain management. Integrated care models that facilitate collaboration among primary care providers, pain specialists, mental health professionals, and other healthcare professionals are essential for optimizing patient outcomes.
By understanding the underlying mechanisms of chronic pain and exploring diverse treatment options, healthcare providers can develop individualized and multimodal approaches to pain management that address the complex biopsychosocial factors contributing to chronic pain and improve the quality of life for individuals living with this challenging condition.